It Takes Two to Tango
The ability to conceive a child naturally has become increasingly challenging for many couples in the UK and the rest of the developed nations. As a result, the demand for assisted reproductive technologies like in vitro fertilisation (IVF) has risen dramatically in recent years. One of the principle causes is a poor diet, this claim might seem nonsensical, but bear with me, the evidence and the science shows why. I will explain how everyone can take some simple steps to optimise their potential to get pregnant, which is not based around weird routines and magic bullets, just simple easy to undertake changes to lifestyle that even the busiest of people can manage.
Causes of Infertility
Infertility affects up to 1 in 7 couples in the UK.[2] It is defined as the failure to achieve pregnancy after 12 months of unprotected sexual intercourse.[3]
The Core Reasons
Infertility can be attributed to female factors (around 50% of cases), male factors (20-30% of cases), or a combination of both.[1]
I am going to cover the things that do not involve physical challenges like ovulatory disorders, tubal blockages, endometriosis, and uterine abnormalities, which need medical intervention to address.[1][5] What you can control is lifestyle, diet and exercise.
Men don’t often consider themselves to be responsible for pregnancy failure but the evidence shows that male infertility is often linked to low sperm count, poor sperm motility, and abnormal sperm morphology.[3]
Other factors that can contribute to infertility include obesity, stress, age, and certain medical conditions.[2][3]
The Role of Diet in Infertility – the evidence.
There is growing evidence that diet and nutrition play a significant role in fertility for both men and women.[3][4] and although what follows is a generalisation it looks like the modern lifestyle is, again, the main driver of this problem, with most of us just being ignorant of the consequences of a high calorie, low nutrient diet dominated by ultra processed foods.
On the plus side diets high in unsaturated fats, whole grains, vegetables, fruits, and fish have been associated with improved fertility outcomes.[3][4]
Specifically, the “Fertility Diet” pattern, which includes less trans-fat and animal protein, but more vegetable protein, monounsaturated fats, high-fibre carbohydrates e.g oats, and multivitamins, has been linked to a 66% lower risk of ovulatory infertility in women.[4]
Discretionary foods high in trans fats, saturated fats, sodium, and added sugars have been consistently associated with poorer fertility in both men and women.[1][3]
In summary, the research indicates that diet and nutrition are important modifiable factors that can significantly impact fertility for both men and women. Adopting a nutrient-dense, anti-inflammatory dietary pattern may help improve the chances of conception.
The Rise of IVF
To understand this trend better, let’s take a closer look at the data on IVF treatment cycles in the UK over the past decade. The table illustrates the significant growth that has occurred in this sector of the fertility industry.
Growth in IVF Treatment Cycles UK – 2010 -2016
| 2010 | 2012 | 2016 | |
| IVF Cycles | 61,726 | 68,014 | 78,993 |
| Increase from 2010 | 10.2% | 27.9% |
In 2010, there were just over 61,700 IVF treatment cycles performed in the UK. However, by 2016 this number had grown by nearly 28% to almost 79,000 cycles. This represents a substantial increase in the utilisation of IVF as couples seek medical intervention to overcome fertility challenges and achieve their dream of starting a family.
The data paints a clear picture of the growing reliance on advanced reproductive technologies like IVF. As getting pregnant naturally becomes more difficult for many, the fertility industry has rapidly expanded to meet this rising demand.
A word of caution here it may be that more people have simply come forward to opt for this type of treatment, however what is clear is that many more are choosing to do so, and there is a skew in the data to some extent because the NHS was offering IVF from 2012 in certain circumstances, although this support was withdrawn by NICE based on its own research into its effectiveness. What the data does show is there are clearly high levels of demand, and it is increasing which says to me that there is little focus being placed on what the individual can do to enhance their own health in order to increase the chances of a natural pregnancy.
Let’s come back to diet.
First, I am going to cover fat which is the misunderstood nutrient that gets blamed for heart disease and many other problems, it is true the wrong fats are drivers of long term non communicable diseases and they make up the majority of fats in the diet, however they can be avoided with a bit of knowledge, or their effects mitigated with some careful supplement additions.
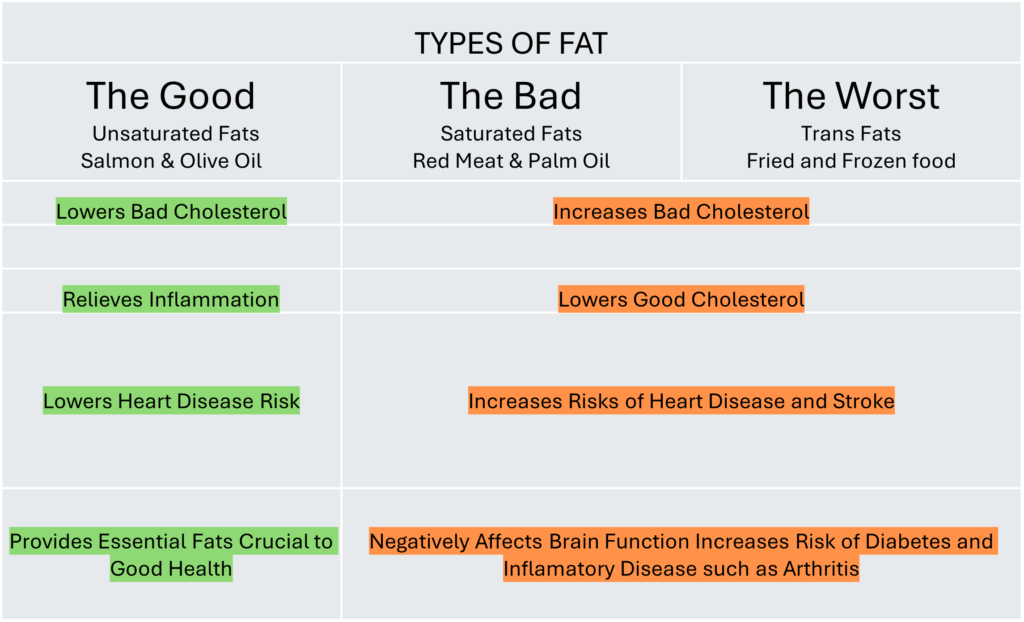
The key differences between good and bad fats are:
Good Fats:
Monounsaturated and polyunsaturated fats, including omega-3 and omega-6 fatty acids, however too much Omega 6 is a problem given its metabolic function in triggering inflammation. They are found in plant-based oils, nuts, seeds, avocados, and fatty fish like salmon, although not farmed salmon, their Omega 3 levels are very low because of the what hey are fed. They help to lower LDL (“bad”) cholesterol and raise HDL (“good”) cholesterol. Their health benefits are extensively researched and known to be crucial, especially the Omega fats which must be got through diet and are essential.
Bad Fats:
Saturated fats and trans fats, such as margarine. They are found in animal products, fried foods, baked goods, and processed snacks. They increase LDL (“bad”) cholesterol and decrease HDL (“good”) cholesterol. Trans fats are particularly problematic, they are solid at room temperature, unlike the liquid good fats, and they are linked to increased risk of heart disease, stroke, diabetes, and other health issues that are driven by inflammation like arthritis.
It is tough to know how much of each type of fat is in your diet, especially as it is often impossible to determine given modern dietary habits, but their are ways to mitigate their effects by supplementing properly and being a little more mindful.
Optimising Fertility
For any couple struggling to get pregnant the first place to start is the store cupboard and freezer to evaluate your everyday diet and asking some hard questions about what your diet is really like. It is well known that everyone needs the Omega Fats, but their importance in the pregnancy process is even greater than people imagine. Omega-3 fatty acids are often hailed as nutritional powerhouses, renowned for their many health benefits. Beyond their well-documented roles in cardiovascular health and cognitive function, omega-3s especially wield considerable influence over reproductive wellness, playing pivotal roles in both male and female fertility. It takes two to tango and both partners need to be involved in ensuring an adequate intake and a proper balance between Omega 3 and 6.
Supporting Male Fertility: The Role of Omega-3 EFAs
For men, omega-3s directly affect sperm production and vigour. Studies have unequivocally demonstrated the correlation between omega-3 levels, particularly docosahexaenoic acid (DHA), and sperm health. Low levels of omega-3s have been linked to poorer sperm quality, diminished motility, and reduced concentration, all of which are critical determinants of male fertility.
Inflammation is a common adversary in the realm of male fertility, capable of wreaking havoc on sperm cells. Omega-3 fatty acids are potent anti-inflammatory agents, providing a protective influence to subdue inflammation and create a more conducive environment for sperm development and function.
The most deficient EFA is Omega 3. Most of the world’s people don’t eat enough oily fish like wild salmon, anchovy, sardines, and mackerel. Extensive testing shows a deficiency in the global population with it being worst in the advanced nations.
Empowering Female Fertility: Omega-3s and Women’s Reproductive Health
In parallel, omega-3 fatty acids wield profound influence over women’s fertility, exerting beneficial effects across various stages of the reproductive process. From regulating menstrual cycles and optimising ovulation to enhancing egg quality and nurturing a healthy uterine environment, omega-3s play multifaceted roles in supporting female reproductive wellness.
Inflammation can disrupt the delicate hormonal balance necessary for regular menstrual cycles and timely ovulation. By mitigating inflammation, omega-3 fatty acids help restore harmony to the reproductive system, promoting regularity in menstrual cycles and optimising the timing of ovulation, thus enhancing the likelihood of successful conception.
Enhancing Egg Quality and Uterine Health for Pregnancy Success
High-quality eggs are essential for successful fertilisation and embryo development. Omega-3s contribute to the maintenance of egg integrity, ensuring optimal conditions for fertilisation and subsequent embryonic growth. Furthermore, omega-3s support uterine health, fostering a nourishing environment for embryo implantation and reducing the risk of early pregnancy loss and complications.
The real challenge is in getting enough Omega 3 from bioavailable sources in the modern diet, which is dominated by ultra-processed foods, in turn this directly causes consistent low-grade inflammation that directly affects both sexes. A perfect storm when trying to get pregnant.
The last word.
The EFAs aren’t the only nutrients that have an impact, it almost goes without saying that vitamins, minerals, and fibre also help to optimise the body. Much of those are obtained through diet but there is no certainty given the quality of a modern diet. My personal experience is the most effective first step towards a healthy body is to get the cellular balance right through the right balance of EFAs, after all they impact every one of the 37 trillion cells that we all have! Get them right and magic happens.
The simplest way for you and you partner to check whether you are deficient is to take a simple, cost effective blood spot test and check the ratio of your EFAs. A quick and informative solution to knowing whether you stand a decent chance of getting pregnant and fulfilling the delivery of the most precious of gifts, a new life.
Contact me for more information.
Citations:
[1] https://academic.oup.com/humupd/article/29/6/811/7226236
[2] https://www.bda.uk.com/resource/a-clinical-update-on-diet-and-fertility.html
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6079277/
[4] https://www.eatright.org/health/pregnancy/fertility-and-reproduction/fertility-foods
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8634384/






